Trending Now
- 830 voters names go missing in Kavundampalayam constituency
- If BJP comes to power we shall consider bringing back electoral bonds: Nirmala Sitaraman
- Monitoring at check posts between Kerala and TN intensified as bird flu gets virulent in Kerala
Columns
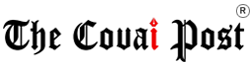
What you can learn from a bonesetter with a BUMS (yes, really) degree
![]() June 25, 2016
June 25, 2016
An excerpt from a book that tracks practitioners of traditional forms of medicine – in modern day India.
Gulam Mohideen was the bonesetter listed on the signboard with the letters BUMS (Bachelor in Unani Medicine and Surgery) after his name and was junior only to his father, Hakim Gulam Rasool. Aged forty-five and having worked in the family clinic since he was a young teen, Mohideen now ran a series of bone-setting practices around Hyderabad.
Called Luqman Clinics after an Ethiopian former slave said in the Koran to have been given a gift of healing wisdom by god, the room we sat in was the oldest treatment centre. The newest (and largest) was to be a hospital on the other side of town, a modern, custom-built structure with an outpatient department as well as beds to accommodate inpatients. The other clinics had better provision for using modern anaesthetics, in which Mohideen had taken a postgraduate course. “I am the only bone setter with a Unani and a higher medical qualification in Hyderabad,” he told me. “I wanted to integrate anaesthetic injections to reduce severe pain.”
Mohideen told me how in his father’s heyday, until the 1970s, bone setters had the opportunity to apply to become Registered Medical Practitioners, or RMPs.
In the days before AYUSH existed as an official denomination, this meant that doctors unqualified in Western medicine could receive legal sanction to practise within their systems, although they were not university-educated. “But many people didn’t know how or didn’t bother, because, like my father, they had already been practising independently and developing bone-setting techniques for many years,” he said.
For Hakim Mohideen’s family, many years actually meant nine generations. His father’s ancestors had come from Delhi as royal physicians in the entourage of the Mogul emperor Aurangzeb, who, in 1687, besieged and destroyed Golconda, the fort about seven miles from Hyderabad, then thought to be one of the most impregnable in south Asia. That particular siege lasted eight months in a period of Indian history in which wars were a regular occurrence, with various battles fought between the Mughals, Persian, Indian, British and other rivals over the years. Battles – on the backs of horses, elephants, or on foot – meant injuries to soldiers, injuries that needed skilled doctors, working under the patronage of their rulers.
The financial security and freedom the trusted hakims were given allowed innovations in treatment to continue in the Gulam family under the reign of the first Nizam, who took over from 1724 when Mughal rule collapsed. The family knowledge of bone manipulation and bandaging as well as plants, potions and pain relief had been passed from father to son in a continuous line.
In the small clinic in which we sat, as well as from the medical supplies in the glass cabinets, there were two large bowls of lep (herbal balm) placed on the floor, which were also part of that tradition. One was white, the other yellow. I knew not to ask what was in them – they are often closely guarded family secrets, made with ingredients that vary between practitioners.
Hakim Mustafa described the basics to me anyway. “The formulation of these leps are from generations back. The white lep is for massage; the yellow is good for pain. Its base ingredients are beeswax and oils, but for different problems, we will make different formulations.”
“All home-made. We don’t market them so there’s no certification,” Hakim Mohideen added.
To his mind, as a BUMS-certified physician, bone setting was not an “alternative” practice but one that fell under the remit of Unani, regulated by the Department of AYUSH. Hakim Mustafa described to me some of their other treatments, including 200 types of tablets, some with calcium, for example, to support bone healing; others, he said, would make the bone soft.
“People come here with every orthopaedic problem – fractures, also rickets, osteoarthritis, cervical problems…We open between eleven in the morning and nine at night, but if any patient needs me for bone fractures or dislocations after that, we attend emergencies also.”
The small room in which we sat was where everything happened, but at three o’clock, in the lull during the hottest part of the afternoon, it was empty. I couldn’t imagine the small space bulging with the sixty to seventy patients I was told attended daily. “There were fewer people coming in my father’s days,” Hakim Mohideen said. “The population is higher now. Everyone comes, now only maybe ten per cent speak Urdu [indicating an Islamic tradition]. We set the bone in seconds, but generally we spend fifteen to twenty minutes with each patient. It’s not just the treatment that takes time. When someone breaks a bone, there is an imbalance of heat. Their lifestyle needs to be adjusted, they must have dietary restrictions.”
Hakim Mustafa spoke more about the akhlat – Unani humours – applying Unani theory to conditions relating to the bone. “People with more bile also have more heat – they are given a different diet – but only until they get well.” I thought back to the carrots, radishes and onions that formed the ingredients of the tablets found on the ancient Greek shipwreck. For Unani, just as for Hippocratic doctors, medicine starts with what we eat and is intimately linked with diet.
“There are more people in Hyderabad now than in your father’s day,” I commented, “but don’t more people today go to Western medical clinics now?’
“For surgery they go to MBBS doctor. For every other fracture they come here,” Hakim Mohideen said. “If they are poor people, they obviously come here. Even rich people come here if their MBBS treatment wasn’t done properly. Bone setting uses movement during therapy, while allopathic treatment means patients need to also go for physiotherapy afterwards.” In such a system, the extra appointments required after the bone is set translated into extra expense that would have to come out of the pocket of patients – as do eighty per cent of healthcare costs in India. Add to that time spent out of paid work while immobilised in a cast and the costs of travelling to and from the hospital, and the prospect of going to an orthopaedic surgeon in the first place would simply not be a viable one for many patients.
“And what do allopathic doctors think of your medicine?” I asked.
“Doctors know us, they say if it’s the Rasool family they don’t mind. There are no other families here that
have as much experience as us,” Hakim Mohideen told me. “Without an X-ray, just by touching we can say whether it’s a break or a fracture. But if we see that someone needs it, we will refer them to have surgery. For example, we do not treat injuries to the femur, because we simply cannot feel it well enough, because of its deep position in the leg. We will tell the patient, go to the diagnostic clinic, take an X-ray. “There are people who set up as bone setters who don’t know what they are doing. Sometimes we have assistants – people who hold the patient while we are locating the bone. Some assistants look at what we do and think that it looks easy – they leave here and set up their own shop. But they have no experience.’
Just then, the afternoon lull broke and the patients flooded in. Hakim Mustafa, who was looking somewhat bored and disgruntled, burst into life as people arrived. The hakims, I could see, were passionate about their work – the change in the room was palpable as the first in line hobbled in with foot pain. He sat on the floor in front of Mustafa and the hakim methodically probed the foot with his fingers and thumb before pronouncing that a tarsal had been dislocated.
Without warning, Hakim Mustafa gently pushed the tarsal as the young man’s face tensed in raw agony for just a few seconds. When he relaxed again, seemingly at ease, he placed Rs 200 on the floor in front of him as the hakim applied lep from one of the giant bowls, bandaged the foot and, with a reel of white thread, expertly sewed the edge of the fabric together.
“Patients come afterwards once a week for about six weeks,” the hakim said as the small room filled with people. “Children heal faster; for them it normally only takes ten to twenty days.”
The next patient the hakim saw had turned up for his sixth appointment – a twenty-two-year-old who had been visiting Luqman Clinic every four days over the previous month. “It was a total break of a metacarpal,” the hakim told me as he placed the man’s arm on a large wooden block.
“How did you do it?” I asked.
“I punched my car window.” He smiled. “I was angry.’
The hakim asked if he felt better and he said that he did. He was no stranger to the clinic, despite (or perhaps because of) his youth. He worked as a personal trainer and his body-building regime had led to several minor muscular injuries over the years, but he first came to Luqman after jumping out of a window and breaking his wrist.
“I did go to the doctor for an X-ray,” he told me, “but I had been told that these hakims were good, so I came here for treatment instead.’
Excerpted with permission from In The Bonesetter’s Waiting-Room: Travels Through Indian Medicine, Aarathi Prasad, Profile Books.
Aarathi Prasad